Quantified self, mHealth and wearable technology. While you could hear about those trends in the past, the tipping point has been reached at the CES 2014. What was supposed to be the future is our present much faster than industry expected. Enterprise market is again far behind consumers. Health care industry tethered by regulations just cannot catch-up quickly enough.
At K-message however, we can take a look at the forefront of the consumer technology and assess its possible impact on the industry, and our focal point – pharmaceutical marketing. But first, let us define what we are talking about.
What is quantified self? Who wears technology? What is mHealth?
Quantified self (QS)
Quantified self (QS) is a trend of personal data collection via technology. The idea is to acquire data on person’s state, actions and performance using wearable technology and/or mobile applications.
Wearable technology is a description of any electronics that one can wear. It may be something with a sensor for quantified self purposes, but it can be also a T-shirt with LEDs intended just to look nice. From quantified self perspective, wearable technology is a trend that enables the whole movement by devices that can capture personal data.
mHealth is a general term for usage of mobile devices (mobile phones, smartphones, tablet computers etc.) in connection to medicine or health care. mHealth includes providing information to the patients or HCPs, but also collecting patients data.
Is Quantified Self big and mature enough to have an impact on health care industry?
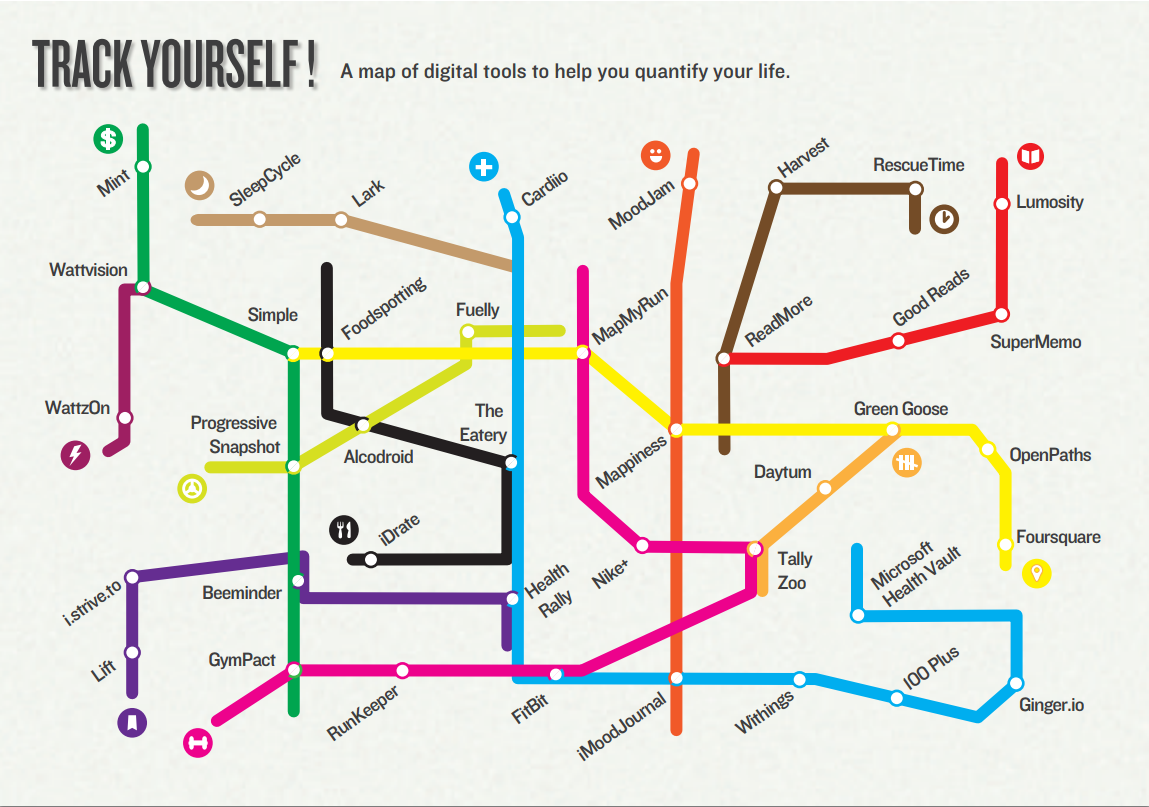
The topic is huge. On the Quantified Self Guide – a website that collects different Quantified Self applications, there are 505 different tools listed at the time of writing this article. Of those 65 are tagged with medicine and 124 with fitness category tag. Wearable technology was main topic of CES 2014. If you look around in the office of any healthcare corporation (or, even better, on the jogging path) in the developed world, you will notice wearable sensors in form of bracelets, chest bands or small items in the shoes used by increasingly high population. Users of the smartphones install “measuring” applications on their devices.
What are the numbers? Runtastic, a mobile app dedicated to track running performance has recorded 60 million downloads worldwide and 25 million registered users on Runtastic.com. Similarly targeted device and app Nike+ platform claims 18 million users. Fitbit.com, the website that allows to see the results of tracking with Fitbit range of devices according to Quantcast has around 2 million users from the U.S. only. Quantified Self is definitely mass market now and it will not fade away. Instead it seems it will get more devices and applications as the tech industry embraces it.
Quantified self: dangers versus benefits
From the pharma marketer perspective quantified self may be even more disruptive than the raise of social media (which, by the way is still not accommodated properly). As it gives more knowledge to the user it takes away control from the HCPs. Fitness trackers are obviously beneficial as they encourage the best prevention against disease – exercise and movement. On the other hand the trend brings some risks with it.
Interpretation of the data gathered by the device or application, even if supported with some mHealth resource filled with scientifically proven knowledge may lead to wrong decisions. Innocent life-logging app that counts calories intake may lead to starvation, or at least to non-balanced diet for some users who want to lose weight too quickly (not mentioning here eating disorders). A non-calibrated blood pressure and pulse tracker may put people with cardiovascular issues at risk (I cannot breath but the reader says I can still run…). The device alone can affect users health by allergy (that happened with Fitbit Force recently), heat, permanent exposure to radiation. There was also at least one occurrence when using activity tracking device, and competing for better score was connected with a tragic death of one too motivated biker.
In pharmaceutical industry there is a lot of pressure put on the patient data privacy. Quantified self puts those data in open, sharing the very personal information on the activity publicly, sometimes without informing user about it. This was a real case when Fitbit.com allowed public to see users who were logging their 30 minutes very active sexual encounters.
What is fascinating in Quantified Self movement is how the application can change focus from empowering by giving the knowledge to the patient to enslaving by enforcing control over users behavior. In one of the quantified self business use cases, not related to health care, a QS device called Hitachi Business Microscope worn by office workers was mapping their communication patterns within organization, pinpointing unnecessary meetings, organization social graph and communication issues.
If we take it to the field of pharma marketing, QS may be seen as a great tool to improve patient compliance or to provide personalized healthcare, but also as a menace of higher insurance rates for any misbehavior – be it sitting too long on the couch or having one drink too much.
Quantified self and EHR, EMR and PHR solutions
One of the promising features of the quantified self is possibility to include the data acquired by sensors directly into electronic health records systems (EHR). Electronic Health Record is not exactly what industry widely embraces as EMR – electronic medical record. Although the data gathered, stored and processed in EHR are more or less the same, the source is different. EMR can include only data provided by medical institutions and healthcare professionals.
EHR is open to any source of data. It includes what can be gathered from EMR, but also accepts patient input, quantified self devices and applications feeds and other sources. A specific range of EHR, that includes only data provided and managed by the user (in this case – patient) is Personal Health Record (PHR). The most renowned solutions of this kind are Google Health (decommissioned) and Microsoft Health Vault, but there are also other providers.

This brings new opportunities as we get really Big Data in EHR, but also some risks. Data in EHR and PHR cannot be really trusted, as they come from not validated sources and can be contradictory. The sampling (how often you take a data point) is not standardized and quality of the input is questionable. Nowadays, adoption of EHR and PHR is very limited, as is their functionality and usability. However with the growth of the quantified self we can expect rising importance of such hubs for the medical information.
Quantified self and regulatory compliance: HIPAA and HITECH
Quantified self movement adoption is nowadays limited to developed nations, and the biggest market for those solutions is in the United States of America. There are two regulatory bodies in the US that overlook quantified self devices and applications. For non-medical use the main authority is FTC. Privacy and access to the health related data is regulated by HIPAA and HITECH regulations.
HIPAA Compliance Checklist
- Have you formally designated a person or position as your organization’s privacy and security officer?
- Do you have documented privacy and information security policies and procedures?
- Have they been reviewed and updated, where appropriate, in the last six months?
- Have the privacy and information security policies and procedures been communicated to all personnel, and made available for them to review at any time?
- Do you provide regular training and ongoing awareness communications for information security and privacy for all your workers?
- Have you done a formal information security risk assessment in the last 12 months?
- Do you regularly make backups of business information, and have documented disaster recovery and business continuity plans?
- Do you require all types of sensitive information, including personal information and health information, to be encrypted when it is sent through public networks and when it is stored on mobile computers and mobile storage devices?
- Do you require information, in all forms, to be disposed of using secure methods?
- Do you have a documented breach response and notification plan, and a team to support the plan?
If you answered no to any of these questions you have gaps in your security fence.
If you answered no to more than three you don’t have a security fence.
Quantified self and regulatory compliance: FDA guidance on medical mobile applications
For medical mobile applications relevant authority is the FDA. The Agency considers mobile phone as a medical device as soon as it meets one of the following:
- It works expressly for medical purposes and offers medical or health-related apps
- It acts as an effective accessory or component to aid medical health
While assessing medical mobile applications the FDA applies the same risk-based approach as for other medical devices. The guidance document provides examples of how the FDA might regulate certain moderate-risk (Class II) and high-risk (Class III) mobile medical apps. The guidance also provides examples of mobile apps that are not medical devices, mobile apps that the FDA intends to exercise enforcement discretion and mobile medical apps that the FDA will regulate in Appendix A, Appendix B and Appendix C.
For many mobile apps that meet the regulatory definition of a “device” but pose minimal risk to patients and consumers, the FDA will exercise enforcement discretion and will not expect manufacturers to submit premarket review applications or to register and list their apps with the FDA. This includes mobile medical apps that:
- Help patients/users self-manage their disease or condition without providing specific treatment suggestions;
- Provide patients with simple tools to organize and track their health information;
- Provide easy access to information related to health conditions or treatments;
- Help patients document, show or communicate potential medical conditions to healthcare providers;
- Automate simple tasks for healthcare providers; or
- Enable patients or providers to interact with Personal Health Records (PHR) or Electronic Health Record (EHR) systems.
Note, that PHR and EHR systems are not covered by the guidance on medical mobile applications.
Here you can see the list of examples of mobile medical applications the FDA has cleared or approved.
This is the list of examples of mobile medical applications for which the FDA will exercise enforcement discretion. Those applications may meet the definition of medical devices but they pose a lower risk to the public in the Agency’s view.
Quantified self: issues to resolve
The quantified self will gain more importance in the healthcare industry. However, there are still some issues to be addressed before embedding them in the marketing strategy. Before building your own application or choosing one from the market consider them carefully.
Tracking versus privacy
Regardless of HITECH privacy considerations, the pharmaceutical company has to be extremely careful about patient data privacy. It has to be absolutely clear to the patient and the organization, that all data are owned by the user of the application and not the company. You need to have users’ direct consent if you are going to aggregate, store, process, or use the data in any way.
Data reliability
Your quantified self-application or device will gather data in connection to patients’ health. Therefore it is important to achieve possibly high level of accuracy and ensure the integrity of this data. It should be also clearly stated what are limitations of the sensors and technology used.
Fallback in case of failure
You need to make sure that in case of failure or loss of the device, patients will still be able to be treated or diagnosed with a fallback solution.
Interoperability
If your application allows data exchange with EMR, make sure it uses open standards, so that it can be used regardless of the health care provider chosen by the patient. This applies also to interoperability with PHR solutions.
Clear guidance for the interpretation of data
Make sure that the data gathered and provided to the patient are not subject to misinterpretation. There should be a clear explanation of the result provided, and if not possible the instruction should point the patient to the HCP who will be able to interpret the data. Even the best result on the application should not encourage patients to be not compliant with the treatment ordered by his doctor.
Co-operation with HCPs
If every patient comes to his GP with gigabytes of life-logging data, there is no time for a proper diagnosis. Valuable information will be hidden in the noise like a needle in a haystack. Not to mention different UIs of the applications and general annoyance with non-standard requests coming out of the blue. To avoid this you need to provide HCPs with clear instructions on what to look for and make sure they will know it at the first glance. Think about a separate dashboard for the physician or even better – distribute the app through the trained HCPs.
Example of quantified self in pharma marketing: Eli Lilly’s Talking Progress.

Talking Progress (this name applies for UK & Ireland markets) is an application available for iOS and Android, that was presented by Claire Perrin on the recent Social Media in the Pharmaceutical Industry conference in London.
Talking Progress is dedicated for adults suffering from depression. Using this app patient can record his/her mood to produce progress charts which can track the recovery and help inform discussions with the doctor. It is extremely important, as one of the symptoms of depression is lack of focus and gaps in the memory.
The app also contains useful hints and tips about lifestyle changes as well as information on causes of depression and treatments.
Talking Progress Features:
- Educational information about depression
- Mood Diary
- Note pages
- Healthy living advice
- Medicine reminder alarm
Together with an app Lilly provides a booklet for the patient and small information desk stand for the HCPs. Embedding quantified self elements (diary and note pages) with mHealth features (educational information, lifestyle advice and compliance reminder) makes this app a perfect companion for patients suffering depression. Providing HCPs with the information pack (they are supposed to “prescribe” an app) guarantees that the data gathered via the app will be used and understood by the doctor.
Quantified self in pharma marketing – an opportunity for everyone
It looks like the quantified self movement will stay with us for longer. Lilly’s example described above shows that properly used it may be beneficial for all – patients, HCPs and pharmaceutical industry. We can without doubt add payers to the list. Correctly applied quantified self is great way for prevention via changing lifestyle habits, increasing disease awareness and improving patient’s adherence to the prescribed treatment. Will we use this opportunity? Quantified self may save lives and money. It seems that even regulatory bodies are up to date with the trend, so the only thing missing is pharma marketers involvement. Do you plan to include quantified self and mHealth elements in your brand strategy?
