Where the regulations help, the funding flows, and the pilots don’t take geological time
If you ask ten founders where to launch a healthtech startup in Europe, eight will say Berlin, one will say London, and one will whisper Lisbon for “quality of life reasons”. They’re all partially right and all are missing the bigger picture.
Europe isn’t one market. It’s 27 regulatory fiefdoms, three reimbursement philosophies, and a few hundred interpretations of GDPR. Your success depends less on your pitch deck and more on which country actually wants what you’ve built.
Below is your 2025 market map, written for people who need real answers: founders choosing their first market, investors analysing expansion, and operator-types who enjoy pain.
1. France
The most healthtech-friendly major market in Europe
Why France works
- Strong government buy-in for digital health.
- Funding muscle: Bpifrance, EU4Health, France 2030.
- Single-payer structure = easier national rollout.
- PECAN (the DiGA-like pathway) actually works.
Best for
Digital care delivery, AI diagnostics, practice management, DTx reimbursement plays.
Funding & Launchpads
- Bpifrance → https://www.bpifrance.fr
- Horizon Europe (FR heavy participation) → https://research-and-innovation.ec.europa.eu
- Paris Santé Campus → https://parissantecampus.fr
Example Startup
Doctolib Valuation: ~€6.4B
The poster child of French digital health integration.
Caveat
French bureaucracy moves fast, but only after explaining for 6 months why it cannot. Labour laws are very strict and unions strong.
2. The Nordics (Sweden, Finland, Denmark)
Small markets, big efficiency
Why the Nordics work
- Public systems open to innovation.
- Culturally high trust → smoother adoption of data-heavy tools.
- A disproportionate number of EU healthtech winners.
Best for
Remote monitoring, diagnostics, preventive health, virtual primary care, health data infrastructure.
Funding & Launchpads
- EIT Health Scandinavia → https://eithealth.eu
- Business Finland → https://www.businessfinland.fi
- Vækstfonden (Denmark) → https://vf.dk
Example Startups
- Oura (Finland) Valuation ~$5.2B
- Kry (Sweden) Valuation ~$2B
- Neko Health (Sweden) Valuation ~$1.8B
Caveat
Great for pilots; too small for scale unless you go south quickly, as Medicover AB and Oura did.
3. United Kingdom
Chaotic, political, commercially attractive
Why the UK works
- One of Europe’s strongest funding ecosystems.
- Private healthcare uptake at record highs.
- NHS validation still opens doors — globally.
- London remains Europe’s top hub for digital health + AI research.
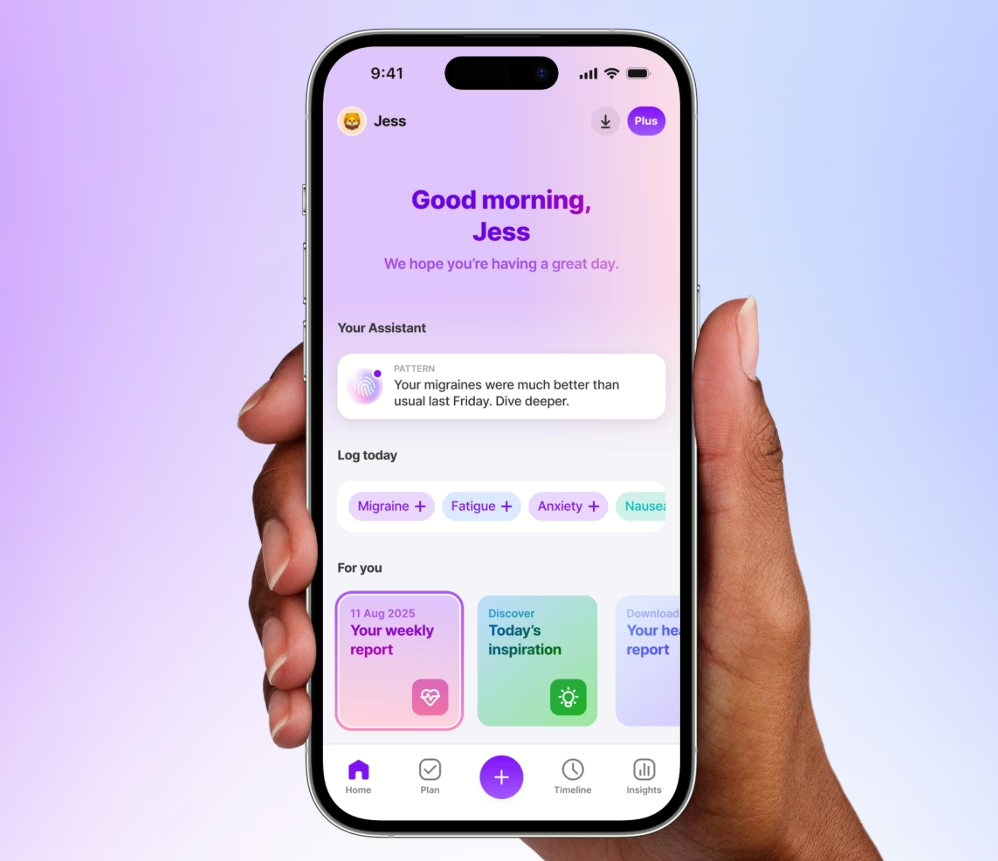
Best for
AI health, care coordination, chronic-care platforms, consumer-forward health apps.
Funding & Launchpads
- Innovate UK → https://www.innovateuk.ukri.org
- DigitalHealth.London Accelerator → https://digitalhealth.london
- EIT Health UK-Ireland → https://eithealth.eu
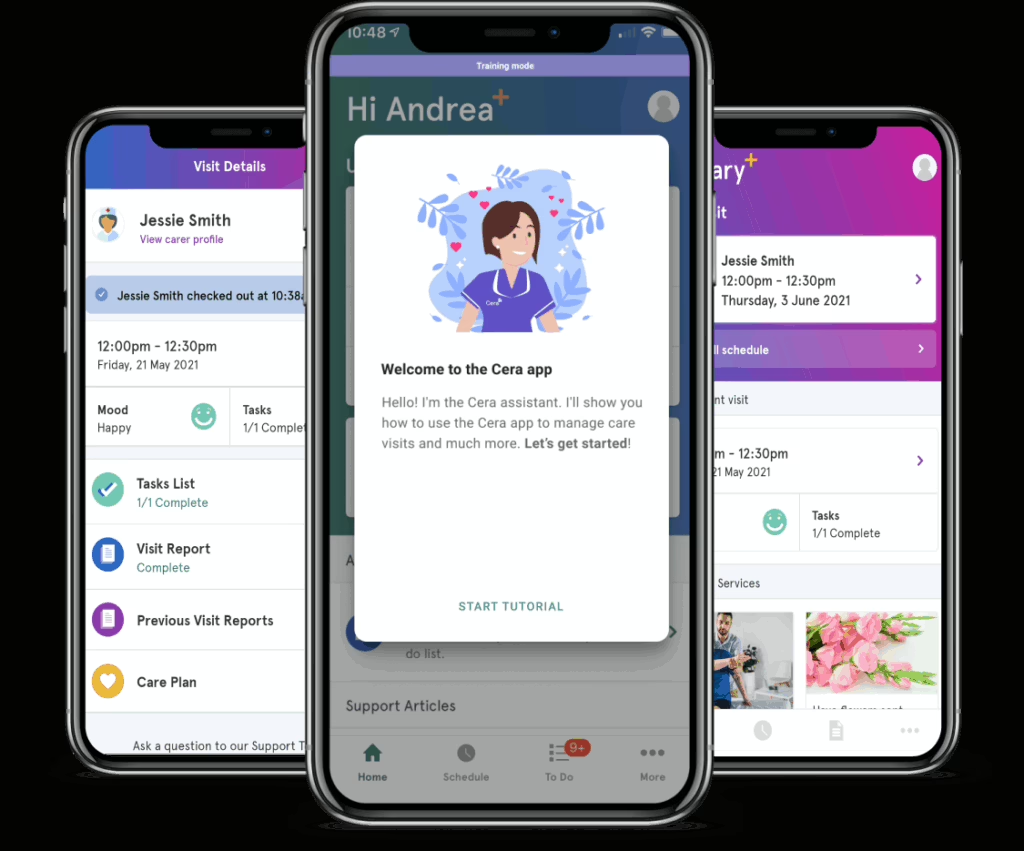
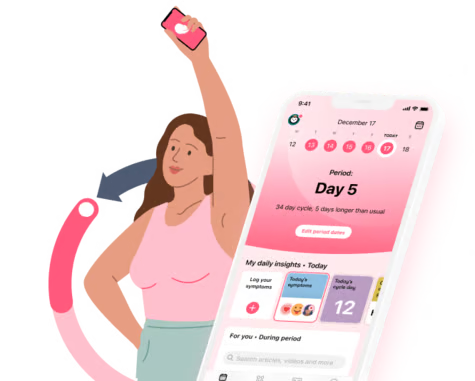
Example Startups
- Flo Health — Valuation ~$1B
- Cera — Valuation ~$1B
Caveat
The NHS is ambitious and inspiring… and also a timeline graveyard. Dual-market GTM (NHS + private) is mandatory.
4. Germany
Complicated, wealthy, occasionally glorious
Why Germany works
- Biggest healthcare budget in Europe.
- Strong reimbursement mechanisms (once you’re “in”).
- Serious medtech and pharma industry footprint.
Best for
Class II/III devices, diagnostics, hospital workflow software, B2B2C employer models.
Funding & Launchpads
- High-Tech Gründerfonds (HTGF) → https://www.htgf.de
- Berlin Health Innovations → https://www.berlinhealthinnovations.com
Example Startup
No German healthtech unicornst that I would be awarte of yet… but Ada Health came close (est. ~$300M valuation).
Caveat
Germany will adopt your product because it is billable and clinically proven, not because it is “innovative”.
5. Spain
Southern Europe’s fastest riser
Why Spain works
- Regional ecosystems (Barcelona, Valencia, Basque Country) punching above their weight.
- Cheaper to operate than Western Europe.
- Private insurers and provider networks actively digitising.
Best for
Chronic-care platforms, elderly-care tech, data platforms, early-stage medtech.
Funding & Launchpads
- KFund → https://kfund.vc
- Barcelona Health Hub → https://www.barcelonahealthhub.com
- Biocat → https://www.biocat.cat
Example Startup
SAVANA Valuation: ~$200M
One of Europe’s most advanced AI/NLP players extracting structured insights from unstructured EHR data. Deployed in 150+ hospitals across 15 countries
Caveat
Spain is a 17-region market. Choose wisely for your regulatory environment and talent pool availability.
6. Switzerland
Small market, big credibility
Why Switzerland works
- Europe’s densest medtech ecosystem.
- Rich reimbursement environment.
- High willingness to pay.
Best for
Device + digital hybrid models, precision diagnostics, biomarkers.
Funding & Launchpads
- Innosuisse → https://www.innosuisse.ch
- Swiss Innovation Park / EPFL Innovation → https://www.swissinnovationpark.ch
Example Startup
Cequr Valuation ~$600M
Wearable insulin delivery.
Caveat
You go to Switzerland for credibility, not market volume.
And now… The CEE Region
The “build-smart, validate-fast” zone investors keep overlooking
CEE is not one region, it’s an efficiency laboratory. If Western Europe drowns you in process, CEE saves you with pragmatism.
Best for
- AI/engineering-heavy products
- Cost-effective clinical pilots
- Digital & device hybrid development
- Workflow automation
- Early validation with real hospitals
Below is the full CEE landscape with funding sources, launchpads and example startups.
Poland. The quiet giant
Funding & Launchpads
- PFR Ventures → https://pfrventures.pl
- NCBR Grants → https://ncbr.gov.pl
- Huge Thing Accelerator → https://hugething.vc
Example:
DocPlanner: Valuation: ~$1.1B
One of Europe’s biggest healthtech exports.
Why it works
Big market, strong talent, private care booming.
Czech Republic – Medtech discipline, startup speed
Funding
- CzechInvest → https://www.czechinvest.org
- HealthCare Lab → https://www.healthcarelab.eu
- i&i Prague → https://www.iniprague.com
Example:
Carebot Valuation: Estimated €8–12M range (seed stage but strong clinical adoption)
AI radiology assistant (clinical decision support)
Why it works
Top-tier clinical research + reasonable procurement.
Slovakia, a tiny market with great AI talent
Funding
- SARIO → https://www.sario.sk
- Laugaricio Ventures → https://laugaricio.vc
Example:
Powerful Medical Valuation: ~$60–80M
AI ECG interpretation.
Why it works
High clinical AI capacity, very open to digital pilot projects.
Hungary, The algorithm factory
Funding
- Hiventures → https://hiventures.hu
- OXO Labs → O3
Example:
Turbine.AI Valuation: ~$80–120M
Virtual cell simulation for drug discovery.
Why it works
Some of Europe’s best AI/ML maths talent.
Romania. The rising talent powerhouse
Funding
- GapMinder VC → https://gapminder.vc
- RoHealth Cluster → https://rohealth.ro
Example:
Telios Care Valuation: ~$20–30M
Telehealth leader for employers and insurers.
Why it works
Massive engineering pool, fast-moving private health sector.
Baltics. Where digital health actually behaves like digital health
Funding
- Startup Wise Guys → https://startupwiseguys.com
- Baltic Sandbox Ventures → https://balticsandbox.vc
Example:
Antegenes (Estonia)
Genomic cancer risk diagnostics (valuation undisclosed, strong EU scaling trajectory)
Why it works
Digital-first culture + world-leading infrastructure.
So where should you start?
If your solution is…
Data heavy → Nordics / Baltics
Reimbursement heavy → France / Germany
Consumer-forward → UK
Hardware + software → Switzerland / Ireland
Cost-sensitive early-stage → Poland / Romania / Spain / Portugal
Europe rewards founders who pick the right first country — not the closest or the coolest.
Start where the system actually wants what you’re building.
Europe HealthTech Market Selection Table (2025)
| Region | Best For | Strengths | Risks / Caveats |
| France | DTx, diagnostics, digital care | Strong reimbursement, centralised system, public funding | Bureaucracy and long cycles |
| Nordics | Remote monitoring, preventive care, data platforms | Fast pilots, high trust, digital literacy | Small markets, must scale outbound |
| United Kingdom | AI health, consumer, care platforms | Strong VC ecosystem, NHS validation, growing private sector | NHS timelines unpredictable |
| Germany | Medtech, diagnostics, hospital IT | Biggest EU health budget, strong reimbursement | Compliance-heavy, slow procurement |
| Spain | Chronic care, elderly care, health data | Lower costs, regional innovation hubs | Fragmented procurement |
| Switzerland | Devices + digital, precision diagnostics | Global medtech hub, strong reimbursement | Small domestic market |
| Poland | Workflow automation, AI tools, B2B | Large population, strong engineering | Regionalised buying, variability |
| Czech Republic | Devices + software, clinical validation | Strong research base, quick adopters | Limited consumer market |
| Slovakia | AI diagnostics, early pilots | High technical talent | Very small market |
| Hungary | AI/ML healthtech, data infra | Top maths/AI talent | Regulatory unpredictability |
| Romania | Telehealth, digital care, SaaS | Large engineering pool | Public sector slow |
| Baltics | Data platforms, interoperability | Digital-first systems, fast pilots | Micro-markets |